
August 19, 2023
Compound Solutions for Feet!
Your feet take a pounding every day, literally. It’s essential to care for those aches, pains, nicks, scratches or infections as they arise but unfortunately, there is no one size fits all solution.
May is Asthma and Allergy Awareness Month in Canada. Spring has sprung. And with it… allergy and asthma season!
When you have asthma or allergies, you must know how and when to use your medicines before a medical emergency. You may have more than one medicine to prevent and treat asthma emergencies when you have asthma.
You can develop an action plan with your doctor or pharmacist, and it will tell you what medicine to use and when. Make sure you are familiar with your action plan to know what to do in an emergency.
How Do I Use an Asthma Inhaler?
When you have asthma, your doctor may prescribe three types of asthma inhalers: long-term control inhalers, quick-relief inhalers and combination inhalers.
A long-term control (also called “maintenance” or “preventer”) inhaler is an inhaler you take every day, even when you are feeling well. It helps keep your asthma under control to reduce your chance of having an asthma episode or attack. These medications work on the inflammation that occurs in the bronchioles of your lungs. This medicine helps you stay in the Green Zone on your asthma action plan. It will not give you immediate relief.

You use a quick-relief (also called “rescue”) inhaler at the first sign of asthma symptoms to keep them from getting worse. You may also take it before exercise or have a cold or other respiratory illness. This medication relaxes the muscles that surround the bronchioles of your lungs when they are constricted or tight. They do NOT reduce the inflammation that is happening. Your doctor will have you take your quick-relief inhaler in the Yellow or Red Zone on your asthma action plan.
Some inhalers have two medicines (called a “combination” or “combo” inhaler) that can be used for both quick-relief and long-term control medicines.
Some people may use a nebulizer instead of an inhaler to take asthma medicines. A nebulizer is a machine that delivers asthma medicine in the form of a mist. This is medication is not more effective than an inhaler; it is just a different way of getting the drug into the lungs for people who cannot coordinate the pressing and inhaling at the same time required of a puffer, such as young children or perhaps they cannot press an inhaler physically as the very elderly.
A nebulizer may not be convenient for travelling because it does take time to inhale the gentle mist to get a total dose. If a nebulizer is not suitable, then an aero chamber and a puffer are quick and effective ways of getting the medication into the lungs.
Many people make mistakes when using their asthma inhalers, even if they don’t realize it. Inhalers If your medicine isn’t reaching your lungs, your asthma might be harder to control, and uncontrolled asthma can make breathing emergencies more likely. Common mistakes that happen over time:
This video shows how you use your inhalers can affect your asthma symptoms. By using them correctly, you can get more medication into your lungs where it needs to go.
How Do I Use an Epinephrine Device?
An epinephrine device injects medicine into your outer mid-thigh. While this device may be easy to use, each type may have a different safety feature, such as a cap you must remove before using it. It would be best to learn how to use the specific device you carry to be comfortable and ready when an emergency happens. If you are unsure, contact one of our pharmacists for more information or a “refresher.”
For additional resources, visit Asthma Canada.
From hormone balance, over gut health, to overall wellness. Stay informed with tips from our pharmacists at Dispensaries Ltd.
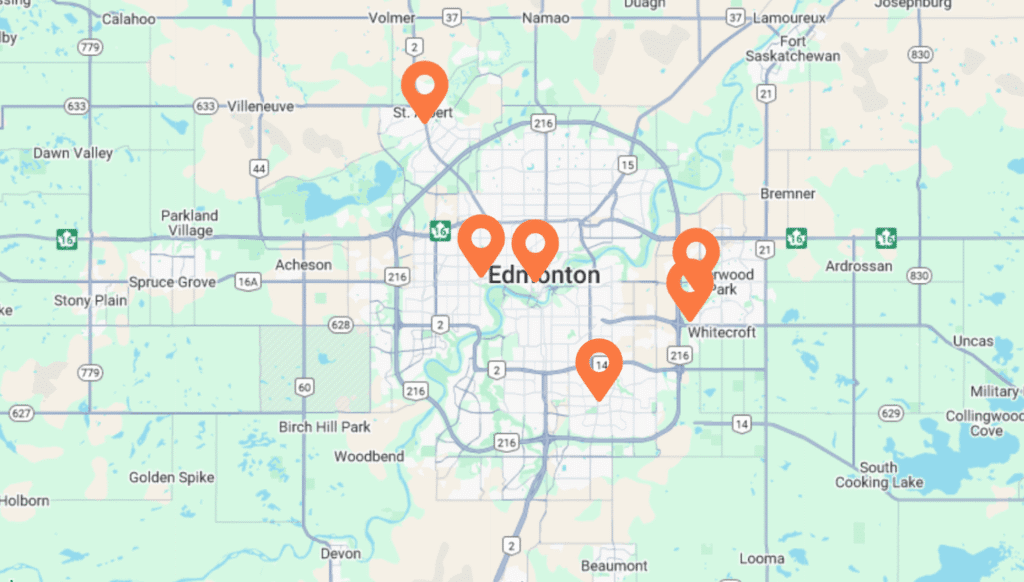
We’re proud to serve communities across the region and throughout Alberta with care and convenience.
Each of our stores is staffed by knowledgeable, compassionate professionals ready to help you with everything from compounding pharmacy services to supplement guidance and beyond.